NOW AVAILABLE ON AMAZON

OUR SUPPLEMENTS LINEUP
At Ladder, we believe high-performance athletes are made, not born, and our goal is to help upgrade performance through better workouts, smarter nutrition, and inside-access to world-renowned fitness experts.
Prep, boost, hydrate, and recover with our supplements
SHOP OUR PRODUCTS ON AMAZON
OUR STORY
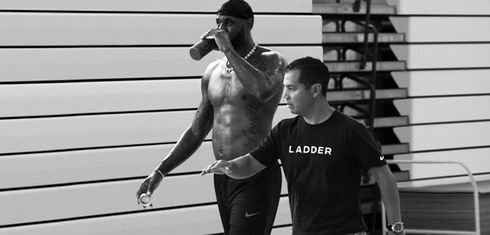
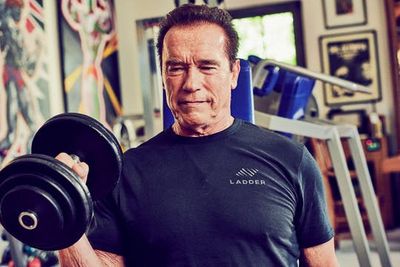
Read about how LeBron James and Arnold Schwarzenegger came together to tackle some of the biggest problems in the supplement world.
OUR STORY
Read about how LeBron James and Arnold Schwarzenegger came together to tackle some of the biggest problems in the supplement world.
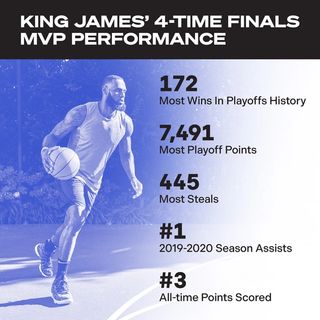
TRUST THE PROS
“When we created Ladder, that was the focus and making sure that everything is clean because that’s what’s more important than anything.”
"With Ladder, we do all the testing so there’s no more guessing about the purity, quality, or effectiveness of protein."
"Focusing on the quality rather than the quantity will allow you to feel satisfied and see the results you deserve!"